Perimenopause - Part 1
What the heck is happening??
WHY IS PERIMENOPAUSE A NEW-ISH PHENOMENON?
Symptoms during perimenopause and menopause could be seen as a side effect of our current culture. Also, it’s EXTREMELY understudied, so we don’t really know how many women suffered in silence for generations.
Even in today’s crazy stressful culture, some women sail into menopause with barely a symptom. So, it’s possible but rare in today’s world. Let’s look at why it’s so rare.
The body struggles to make enough hormone when:
The body is under significant stress.
The diet doesn’t provide enough nutrients.
Physical illness
Too many stimulants (coffee/cigarettes)
Too much alcohol
Relationships that drain all the energy out of her body
It’s not surprising that 75% of women need some help during this transition. You’re not alone; you didn’t do anything wrong—it’s our culture and the lack of support that most women deal with that is to blame.
Hormone Dance – What’s Happening?
Perimenopause, often referred to as the transition period before menopause, can start as early as your 30s but typically begins in your 40s. This phase is characterized by fluctuations in estrogen and progesterone, the two primary female hormones. These hormonal changes are at the heart of many symptoms you might be experiencing.
It seems there are 3 phases of perimenopause (yes, using the word “seems” is appropriate considering the lack of research):
Phase 1 – Low Progesterone
Phase 2 – Estrogen Starts to Swing
Phase 3 – Low Estrogen
Hormones 101
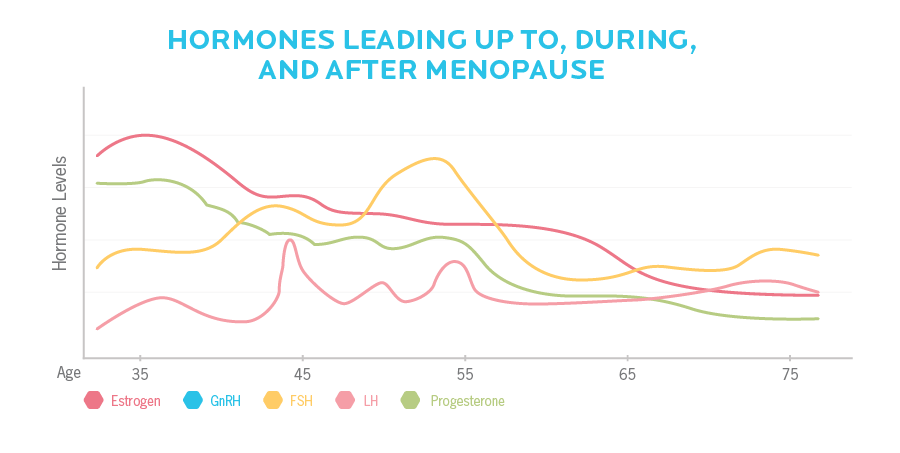
There are 4 main hormones involved in perimenopause: Estrogen, Progesterone, FSH (Follicle Stimulating Hormone), and LH (Luteinizing Hormone).
This is a quick tutorial on these 4 hormones, and I’ll be referring to them regularly throughout this guide:
Estrogen: This is thought of as the “growing hormone” as it stimulates the growth of the uterine lining and helps an egg to mature in the ovaries. It’s produced mostly in the ovaries, but the adrenal glands and fat cells also produce some estrogen. Actually, researchers are finding that estrogen production and estrogen-sensitive cells are found throughout the body.
Progesterone: This is considered the “relaxing hormone” and balances estrogen and its growth potential. It’s mainly produced during the second half of your cycle and reins in the growth of the uterine lining and makes it ready for a possible pregnancy (a.k.a “pro-gestation”).
Progesterone levels are highly connected to the overall stress in your life because cortisol and progesterone share the same precursor.
FSH (Follicle Stimulating Hormone): This hormone is produced by your pituitary gland (in the brain) and stimulates your ovaries to mature an egg.
LH (Luteinizing Hormone): Also produced by the pituitary gland, it stimulates the ovarian follicle to release the matured egg.
Menopause is diagnosed when your FSH rises above 30 mIU/ml and/or when you’ve gone 12 consecutive months without a period.
PHASE 1 – HIGH ESTROGEN, LOW PROGESTERONE
This phase can start anywhere from your late 30s to your late 40s. These hormones are supposed to dance together in a delicate balance, so the drop in progesterone makes the body think it’s dealing with estrogen excess (Estrogen Dominance).
It’s common to notice a change in your menstrual cycle or spotting. You may also have a strengthening of your PMS symptoms, like breast tenderness, or you may develop new symptoms.
Common early perimenopausal symptoms:
Decreased sex drive
Trouble sleeping
Heavy periods
Bloating and water retention
Breast swelling and tenderness
Weight gain around the belly and hips
Cold hands and feet
PMS headaches
Chronic stress will exacerbate this imbalance (more on that in Part 2). Your body uses the same precursor, pregnenolone, to make both progesterone and cortisol. If your stress is high, your body will make much more cortisol and less progesterone. High insulin levels will also make this imbalance worse (see the connection in Part 3).
If you’re considering using hormone replacement at this stage, it’s important to work with a trained practitioner (like a Naturopath or Functional Medicine Doctor) and have an in-depth hormone test (like a DUTCH test). You don’t want to supplement with the wrong hormone, like adding more estrogen when it’s progesterone you need.
PHASE 2 – ESTROGEN STARTS TO SWING
Progesterone levels continue to fade, and now estrogen begins to swing. Your ovaries are trying to mature more and more eggs, so the reserves can get used, and this can increase estrogen levels and increase your risk of a twin pregnancy (watch out!).
This can increase all of your previous symptoms and may cause heavy/long periods. Fibroids may also pop up in this phase. Many of my clients have described this phase as “The Floodgates of Hell” due to long and relentless periods.
PHASE 3 – ESTROGEN DECLINES AND FSH & LH RISE
Your period is becoming noticeably irregular, sometimes skipping months altogether. You’re not ovulating every month anymore, but you can still get pregnant (so be careful).
Night sweats and hot flashes become much stronger and more prominent. They’re a sign of low estrogen and high FSH, which is why this is such a common symptom. Sleep might also become very elusive in these years.
Fatigue, vaginal dryness, low sex drive, and moodiness are also connected with this stage of perimenopause. This is the most common time women seek out hormonal support to help with symptoms.
What happens when estrogen drops?
Estrogen has many jobs in the body outside of fertility. It helps to:
Build and maintain muscle (your muscle mass is important, more on that in Part 2)
Access energy stores in your mitochondria (that’s why you’re tired)
Regulate inflammation (so you have more inflammation)
Increase insulin sensitivity (so the risk of insulin resistance and Type II Diabetes increases)
Balance water stores (that’s why you’re so bloated)
Most women will reach menopause within 1–3 years of reaching this stage.
Since menopause is defined as not having a period for 1 full year and you won’t know when you’ve had your last period until you’ve gone a year without them, this is a very unpredictable time.
The average age for reaching menopause is 51, and it’s commonly reached anywhere between 40–58. Five percent of women reach menopause before 44 and 5% reach it after 55. Ninety percent fall somewhere in between. Your genes can play a role, and there’s a good chance that your menopause age will be similar to your mother’s or grandmother’s, if you have access to that information.
Impact on the Body and Mind
These fluctuating hormone levels impact more than just your reproductive system. Estrogen plays a crucial role in many bodily functions, including mood regulation, bone density, and skin elasticity. As estrogen levels drop, you might notice changes in these areas as well. Here’s a quick rundown of what you might be experiencing:
Mood Swings and Anxiety: Lower estrogen levels can affect neurotransmitters in the brain, leading to mood swings, anxiety, and even depression.
Hot Flashes and Night Sweats: These are classic perimenopausal symptoms caused by the body’s response to hormonal fluctuations.
Irregular Periods: Your menstrual cycle can become unpredictable. Periods might be longer, shorter, heavier, or lighter than usual.
Sleep Disturbances: Changes in hormone levels can wreak havoc on your sleep patterns, making it difficult to get a good night’s rest.
Skin and Hair Changes: Estrogen is vital for maintaining skin elasticity and hair health, so you might notice drier skin and thinning hair.
Understanding what’s happening in your body is the first step towards managing your symptoms. By recognizing that these changes are a normal part of the perimenopausal journey, you can approach them with more patience and less frustration.
Now that we’ve covered the hormonal rollercoaster, let’s move on to some of the specific challenges you might be facing and how to tackle them head-on. In the next part, we’ll dive into why you might be gaining weight despite your best efforts and explore strategies for getting better sleep.
Got any questions or comments? Comment below, jump to our private Facebook Group, or the Ask Lisa page :).